from the Developmental Disabilities Administration
Certified community residential services providers supporting individuals through the COVID-19 crisis
Frequently Asked Questions (FAQ) Third Edition
August 3, 2020
1. How can a provider support clients through the COVID-19 pandemic?
As we continue through these unprecedented times we have all felt the effects of isolation, the inconvenience of wearing a mask and the disruption to our routines. It is important that we support each other to find ways to cope with the drastic changes as well as developing new safe and healthy habits. Providers and clients have likely found ways to cope, but here are some ideas that may help:
-
- Continue to encourage clients to follow the guidelines provided by the Center for Disease Control (CDC) and the Washington Department of Health (DOH). Residential Care Services has also developed guidelines specific to residential settings and can be found at FamHelp Facility Status and Information under Safe Start for Long-Term Care, Full Plan (Certified Community Residential Services and Support). This information was presented at a webinar on July 31, 2020. RCS will be publishing a recording of the webinar if you were unable to attend.
- Provide clients with information in a way they most effectively communicate, on the current situation caused by the virus. There is informational material that has been developed for individuals and families that describe the current crisis. Informing Families has published resources that may be helpful and are available on their website.
- There is a recorded webinar on the DDA COVID-19 site that may be helpful: Home Survival guide with Dr. Phillip Diaz.
- Encourage clients to select activities that allow for social distancing of 6 feet from others, and use of their room to stay away from others to reduce the risk of potential transmission.
- Support clients to make an informed choice by advising them of the risk their choice has to themselves and others.
- Refer to the client’s support plan to see if target behaviors are addressed. Consider applying behavioral strategies to support the client to make safer decisions and comply with the guidance from Department of Health (DOH). If the behavioral strategies in the client’s plan are not successful you may contact the client’s case manager. They can access assistance from the regional clinical team if needed.
2. How do providers support clients to return to jobs and community safely?
All activities in the community should be assessed individually to assure compliance with the Governors current proclamation that gives direction on “safe start” strategies. . This includes employment, community inclusion and any other time spent in the community. Continuing to work or volunteer is an important part of everyone’s lives and must be balanced with health and safety concerns. DDA expects providers to follow the Governor’s directive and evaluate each situation individually as it applies to the County of residence. When considering safeguarding an individual’s personal health and safety, it is important to balance the individual’s right to make their own choices and their personal health and safety.
The client and their support team should work collaboratively to make decisions that best ensures the health and safety of the client, staff and the community at large. The providers should take reasonable measures to mitigate the spread of the virus. If a client is not working or volunteering during this time, assist the clients that you work with to fully explain their absence from their employer and, if applicable, their job support agency. Client may request leave from the employer and convey their interest in resuming their employment after this time of crisis is over. There is a tool being developed called COVID – 19 Return to Employment Services Guidelines that will allow for collaboration between the client and their residential and employment providers.
3. What guidelines are in place for clients visiting their community?
RCS has provided guidance that can be found here: COVID -19: Reopening of Washington State and Client Visits to the Community
4. Has the Governor’s proclamation regarding suspension of training requirements for long-term care workers been extended?
Some training timelines continue to be suspended under the COVID-19 Pandemic State of Emergency Proclamation 20-05 through August 31, 2020. 40 hour CORE, 30 hours of Populations Specific training and Continuing Education Training remain suspended. Providers should continue to offer trainings virtually whenever possible
5. Has the allowance for the 75 hour virtual training been extended?
All of the Train-the-Trainer academies have moved online.
All Community Residential provider trainings are now virtualized with 40 hour CORE Chapter 12 being a hybrid virtual/small in-person skill demonstration sessions with social distancing. Contact Sarah Blanchette for guidance.
Virtualized courses include:
-
-
- Virtualized Train-the Trainer Academies
- CE Series Train The Trainer
- 40 hour CORE Train The Trainer (starting July 2020)
- 5 hour DDA Safety and Orientation training available on the DDA internet site: Community Residential Services Online Training
- 40 hour CORE
- 30 hours of Population Specific training
- Peer Coaching can be conducted virtually or 1:1 with social distancing on-the-job
- Online CPR/First Aid
- Virtualized Train-the Trainer Academies
-
6. What do I do if a new hire cannot get proof of education?
If a prospective employee is unable to locate their High School Diploma, consider substituting other credentials, such as a letter from the school/school district, or transcripts. If the prospective employee is still unable to provide proof, talk with your DDA Resource Manager about requesting an exception to rule. As part of the exception request the provider should submit an attestation from the staff stating that they have graduated from High School or have a GED. When the current emergency ends, the provider must obtain verification of the High School Diploma or GED.
7. What are the nurse delegation requirements currently in place?
Rule changes related to COVID-19 for nurse delegation will be in place through August 31, 2020. These are the current requirements:
-
- Client visits must be completed every 90-120 days.
- One client visit must be competed for insulin delegation—the additional three visits are allowed if needed but the requirement to complete them has been suspended for now.
- Delegated staff must have a current NAR credential.
- Delegated staff must complete 9 hours Nurse Delegation for Nursing Assistant and 3 hour Special Focus on Diabetes if giving insulin. Virtual training is acceptable.
- Electronic signature is valid for consent forms.
8. Can all nurse delegation requirements be temporarily suspended?
Requirements for Nurse Delegation can be met using flexible ways however the training cannot be suspended.
9. Are all Supported Living clients and staff being tested for COVID-19?
The Department of Health is working on a way to test clients served by Supported Living agencies and staff working at client homes while still allowing providers to keep an adequate level of staffing to support the clients. More information about this will be communicated in the future.
10. Why is it important that providers submit information to the online COVID-19 Facility Survey?
The online COVID-19 survey allows RCS to inform public health partners in resource deployment. If providers are underrepresented it may prevent them from receiving the resources they need.
You can find a link to survey here: COVID-19 Facility Survey.
You can find a link to letter here: DEPARTMENT REQUEST FOR ONGOING COVID-19 STATUS UPDATES.
11. How can providers request Personal Protective Equipment (PPE) when they have a client who tests positive?
-
- Providers need to first reach out to their local health jurisdiction (LHJ)
- When conversing with the LHJ, The provider needs to specify that they are providing direct care support for a vulnerable adult when requesting support (testing or PPEs)
- Inform the region, through their DDA Case Manager (CRM)or Resource Manager(RM), they need support
- The RMs/CRMs need to ensure that the SL agency has communicated their need for support to the LHJ.
- The RAs or RMAs will then forward the requests to headquarters.
- Providers need to first reach out to their local health jurisdiction (LHJ)
12. What are the requirements for direct support staff wearing a mask when supporting someone who is not COVID-19 positive?
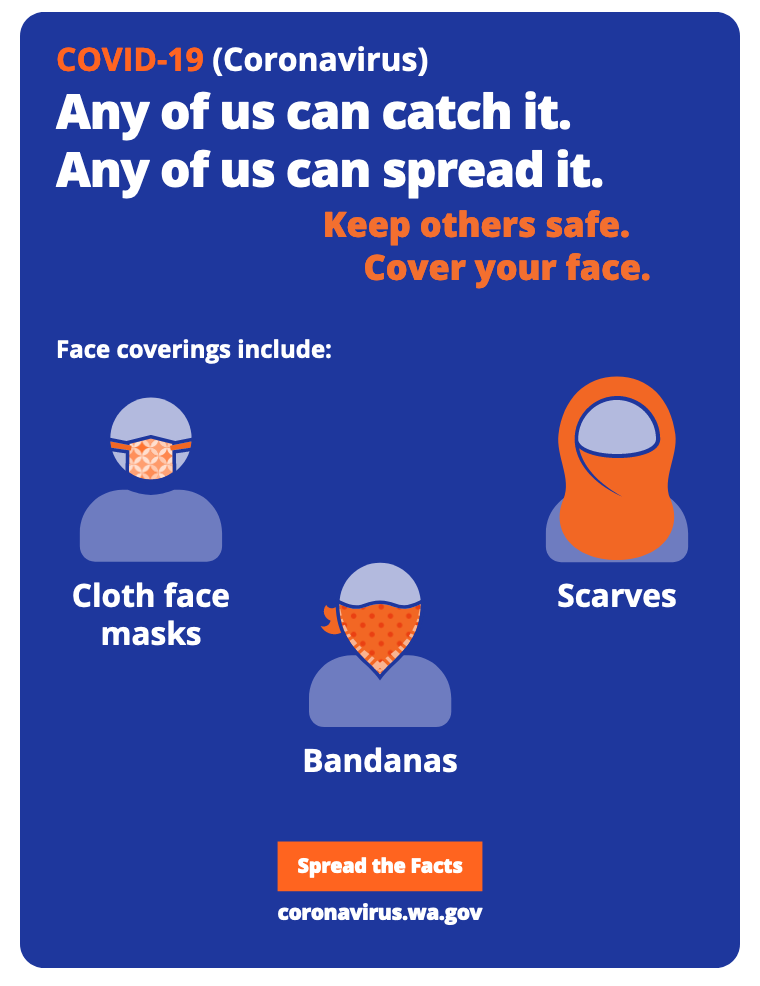
According to DOH guidelines, all staff, regardless of their position must wear a cloth face covering or face mask while in the client’s home if there are currently no COVID-19 positive cases. If there are positive cases additional requirements are needed. If you have questions, your local health jurisdictions may be able to assist you.
13. How can I help the client I support to wear a mask?
Providing clients with information on the current world situation is important. An increased understanding of why they need to wear a mask may help a client to comply with the governor’s order. Also, remember that there are many forms of masks (traditional mask, bandana, balaclava, etc.) Offer choices of face coverings that may be more comfortable for them. Include the client in choosing the mask. A mask with a favorite sports team or color may help.
14. Will Temporary rate increase funds continue past June 30th, 2020 for Supported Living, Group Training Homes, Group Homes, Companion Homes and Alterative Living providers?
Providers received a second rate increase effective August 1, 2020 through September 30, 2020. This increase was calculated to ensure that July 2020 costs were included. These funds are to be used to address unique costs due to the COVID-19 pandemic. Details for supported living, group training homes and group homes can be found here. Details for companion homes can be found here. Details for Children’s Licensed Staff Residential can be found here.
15. If staff are staying in the client’s home during the COVID-19 pandemic, does the provider pay a portion of utilities if live in?
If there are increases in client living expenses, due to the agency staff living in the client’s home, the agency should consult with the DDA Resource Manger to address the costs.
16. Has the monthly premium waiver for Healthcare for Workers with Disabilities (HWD) been extended?
The HWD premium waiver has been extended through October 2020, until the declaration of the public health emergency is due to expire.
17. How do I sign up for a volunteer staff registry that may provide staff support to my agency?
Agencies who want to request approved volunteers, or want to request to activate specific staff under this program as part of their own surge planning, can go to the DOH website under “Facility Instructions for Requesting Volunteers”.
18. Are DDA clients who test positive able to go to COVID only facilities?
We have five Skilled Nursing Facilities that have extended their COVID 19 Cohort Unit contracts with DSHS through September 30th, 2020 in Tacoma, North Seattle, Bellingham, Pasco, and Seattle. Please contact your DDA Case Manager or Resource Manager if you have a client who may qualify.
19. What are the requirements for community protection treatment team meetings?
The requirement for community protection treatment team meetings to be held every 90 days has been waived via Governor’s proclamation. For more details see Governor’s Proclamation.
20. Where can I find information about how many DDA clients and their staff have been effected by the virus?
DDA has data on the prevalence of COVID-19 in community residential services available that can be found here: DDA Community Residential Service Providers with Confirmed COVID-19 Cases.